Have you been hearing of 'herd immunity' very often lately? The pandemic has made these terms extremely popular. But, can it actually protect you from deadly viruses?
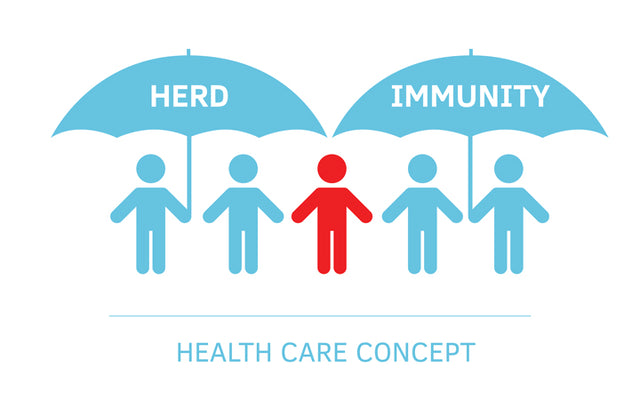
Herd immunity or community immunity is an indirect protection from an infectious disease. It happens when the majority of a population becomes immune to a particular pathogen.
In this article, we tell you all about herd immunity and how it works.
Highlights:
Understanding Herd Immunity
For many bacterial or viral diseases, the pathogen (disease causing organisms) from a diseased person infects another susceptible person (who is not immune to the disease), thereby spreading the disease.
When the majority of a population becomes immune to a particular pathogen through infection or vaccination, chances of disease transmission to susceptible individuals becomes less. This either slows down the spread of the disease or wipes out the pathogen altogether. [1]
Herd immunity can be achieved when a certain percentage of the population acquires immunity to the particular disease through natural infection or vaccination. This is known as the ‘herd immunity threshold’ (HIT).
Let us consider the example of measles which is a highly contagious viral disease. WHO (World Health Organisation) proposed that 95% of the population needs to be immunised to achieve herd immunity against measles in Europe. [2]
This means that if every 19 out of 20 children are vaccinated for measles, the virus cannot infect them or transmit further. The chain of transmission is broken and this may prevent the disease from reaching other susceptible children.
But if a lesser number of children are vaccinated in the population, then the virus can easily pass on to more susceptible children, resulting in a major outbreak.

How Effective Is Herd immunity?
It is important to understand that herd immunity to a particular disease depends on several factors such as
- The contagiousness of the pathogen is i.e, how fast and how easily does it spread,
- And the percentage of immune persons required to prevent the transmission of the pathogen varies depending on the particular pathogen.
For some infectious diseases, herd immunity can be achieved even if 40 - 60% of the population is immune to the disease. But many infectious diseases require 80-90% of the population to be immunised, to achieve effective herd immunity.
Additionally, pathogens tend to mutate over time to escape immunity developed against them. For example the influenza virus mutates over very short periods of time making it very difficult to gain immunity against these viruses.
Also, individual immunity acquired through disease or previous infection guarantees protection during future infections. However, protection through herd immunity depends on multiple factors like
- How evenly distributed is the population in terms of age, living conditions, etc.?
- What are the chances of an infected individual coming in contact with a susceptible member of the community?
Therefore, herd immunity might not be very reliable when it comes to protection from infections.
Most importantly, herd immunity may weaken over a period of time. This may be due to the introduction of new susceptible members into the population through birth, migration, etc., or the loss of immune members due to death from other reasons. [3]
Historical Examples Of Achieving Herd Immunity
The most common and scientifically reasonable way of achieving herd immunity is through mass vaccination. When an individual gets vaccinated, he not only protects himself, but the entire community.
Before the advent of vaccination, herd immunity was achieved through naturally acquired infections. But, it often came at the cost of morbidity and mortality of a large percentage of the population, especially in case of highly contagious diseases.
It has been observed in the past that an effective vaccination schedule can wipe out infectious diseases like polio, smallpox, measles etc. from a particular population. Herd immunity might have played an important role there. It had also slowed down the transmission of infections of pertussis, rotavirus and cholera among others.
However, it has to be kept in mind that the efficacy of vaccination can reduce over time. Also, infected persons travelling from one place to the other can reintroduce a pathogen to a mass immunised population.
For example, the introduction of a single infectious person caused a cholera outbreak in South Sudan camp in October 2016, even though they were mass vaccinated between 2014 and 2015. [4]
Herd Immunity: Pros And Cons
Pros
The most beneficial effect of herd immunity is protecting those with a weak immune system or someone who cannot receive a particular vaccine. For example
- Infants
- Pregnant women
- Elderly with a weakened immune system
- Immunocompromised patients like those suffering from HIV/AIDs, cancer, diabetics, etc.
It is interesting to note that vaccinating kids for pneumococcal diseases had reduced the rate of infection among the elderly in a particular population. [5] Thus, appropriate vaccination not only protects the vaccinated individual from the disease, but also extends protection to the entire community.
Cons
On the downside however, it may not be judicious to rely totally upon herd immunity as an effective means of protection against an infectious agent. Vaccination and preventive measures should be taken whenever possible.
Additionally, there might be a lot of damage caused before herd immunity can be achieved through natural infections. Natural infections can lead to diseases, permanent injuries or loss of many lives before herd immunity is achieved.
Risks Of Herd Immunity
There are a number of risks involved in relying on herd immunity to slow down or prevent an infectious disease outbreak.
We have to remember that the herd immunity threshold (HIT) is a statistical value and not an absolute number. This means that even if the required percentage of the population is immune to a disease, it does not guarantee prevention of transmission of the pathogen.
There are several factors that may affect the extent of protection through herd immunity
- The permanence of the immunity against the pathogen
- The frequency of contact of an infected person with other susceptible members
- Proportion of immune population to susceptible individuals at a given time point.
Also, many pathogens such the Flu virus can mutate rapidly, which makes it particularly difficult for herd immunity to work. Therefore, herd immunity is definitely not an alternative to preventive measures such as vaccination, etc.
Wrapping Up
Herd immunity or community immunity against a particular disease is achieved in a population when a certain percentage of that population is immune to that disease through natural infections or vaccinations. While it is good at protecting the weak or immunocompromised members of a population, it is not a reliable alternative to other prophylactic measures for disease prevention.
Recommended Products
Was this Article helpful?
- Least helpful
- Most helpful